Image above: Kiarra Boulware and her niece at Penn North, an addiction-recovery center in Baltimore
In Baltimore and other segregated cities, the life-expectancy gap between African Americans and whites is as much as 20 years. One young woman’s struggle shows why.
By Olga Khazan, The Atlantic —
One morning this past September, Kiarra Boulware boarded the 26 bus to Baltimore’s Bon Secours Hospital, where she would seek help for the most urgent problem in her life: the 200-some excess pounds she carried on her 5-foot-2-inch frame.
To Kiarra, the weight sometimes felt like a great burden, and at other times like just another fact of life. She had survived a childhood marred by death, drugs, and violence. She had recently gained control over her addiction to alcohol, which, last summer, had brought her to a residential recovery center in the city’s Sandtown neighborhood, made famous by the Freddie Gray protests in 2015. But she still struggled with binge eating—so much so that she would eat entire plates of quesadillas or mozzarella sticks in minutes.
As the bus rattled past rowhouses and corner stores, Kiarra told me she hadn’t yet received the Cpap breathing machine she needed for her sleep apnea. The extra fat seemed to constrict her airways while she slept, and a sleep study had shown that she stopped breathing 40 times an hour. She remembered one doctor saying, “I’m scared you’re going to die in your sleep.” In the haze of alcoholism, she’d never followed up on the test. Now doctors at Bon Secours were trying to order the machine for her, but insurance hurdles had gotten in the way.
Kiarra’s weight brought an assortment of old-person problems to her 27-year-old life: sleep apnea, diabetes, and menstrual dysregulation, which made her worry she would never have children. For a while, she’d ignored these issues. Day to day, her size mostly made it hard to shop for clothes. But the severity of her situation sank in when a diabetic friend had to have a toe amputated. Kiarra visited the woman in the hospital. She saw her tears and her red, bandaged foot, and resolved not to become an amputee herself.
Kiarra arrived at the hospital early and waited in the cafeteria. Bon Secours is one of several world-class hospitals in Baltimore. Another, Johns Hopkins Hospital, is in some respects the birthplace of modern American medicine, having invented everything from the medical residency to the surgical glove. But of course not even the best hospitals in America can keep you from getting sick in the first place.
It was lunchtime, but Kiarra didn’t have any cash—her job, working the front desk at the recovery center where she lived, paid a stipend of just $150 a week. When she did have money, she often sought comfort in fast food. But when her cash and food stamps ran out, she sometimes had what she called “hungry nights,” when she went to bed without having eaten anything all day.
When I’d first met Kiarra, a few months earlier, I’d been struck by how upbeat she seemed. Her recovery center—called Maryland Community Health Initiatives, but known in the neighborhood as Penn North—sits on a grimy street crowded with men selling drugs. Some of the center’s clients, fresh off their habits, seemed withdrawn, or even morose. Kiarra, though, had the bubbly demeanor of a student-council president.
She described the rough neighborhoods where she’d grown up as fun and “familylike.” She said that although neither of her parents had been very involved when she was a kid, her grandparents had provided a loving home. Regarding her diabetes, she told me she was “grateful that it’s reversible.” After finishing her addiction treatment, she planned to reenroll in college and move into a dorm.
Now, though, a much more anxious Kiarra sat before her doctor, a young white man named Tyler Gray, who began by advising Kiarra to get a Pap smear.
“Do we have to do it today?” she asked.
“Is there something you’re concerned about or nervous about?,” Gray asked.
Kiarra was nervous about a lot of things. She “deals by not dealing,” as she puts it, but lately she’d had to deal with so much. “Ever since the diabetes thing, I hate hearing I have something else,” she said softly, beginning to cry. “I’ve been fat for what seems like so long, and now I get all the fat problems.”
“I don’t want to be fat,” she added, “but I don’t know how to not be fat.”

Kiarra resolved to get healthy after visiting a diabetic friend in the hospital who’d had her toe amputated. Kiarra’s own diabetes is already causing her vision to blur. (Jared Soares)
Kiarra’s struggles with her weight are imbued with this sense, that getting thin is a mystery she might never solve, that diet secrets are literally secret. On a Sunday, she might diligently make a meal plan for the week, only to find herself reaching for Popeyes fried chicken by Wednesday. She blames herself for her poor health—as do many of the people I met in her community, where obesity, diabetes, and heart disease are ubiquitous. They said they’d made bad choices. They used food, and sometimes drugs, to soothe their pain. But these individual failings are only part of the picture.
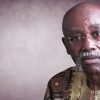
In Baltimore, a 20-year gap in life expectancy exists between the city’s poor, largely African American neighborhoods and its wealthier, whiter areas. A baby born in Cheswolde, in Baltimore’s far-northwest corner, can expect to live until age 87. Nine miles away in Clifton-Berea, near where The Wire was filmed, the life expectancy is 67, roughly the same as that of Rwanda, and 12 years shorter than the American average. Similar disparities exist in other segregated cities, such as Philadelphia and Chicago.
These cities are among the most extreme examples of a national phenomenon: Across the United States, black people suffer disproportionately from some of the most devastating health problems, from cancer deaths and diabetes to maternal mortality and preterm births. Although the racial disparity in early death has narrowed in recent decades, black people have the life expectancy, nationwide, that white people had in the 1980s—about three years shorter than the current white life expectancy. African Americans face a greater risk of death at practically every stage of life.
Except in the case of a few specific ailments, such as nondiabetic kidney disease, scientists have largely failed to identify genetic differences that might explain racial health disparities. The major underlying causes, many scientists now believe, are social and environmental forces that affect African Americans more than most other groups.
To better understand how these forces work, I spent nearly a year reporting in Sandtown and other parts of Baltimore. What I found in Kiarra’s struggle was the story of how one person’s efforts to get better—imperfect as they may have been—were made vastly more difficult by a daunting series of obstacles. But it is also a bigger story, of how African Americans became stuck in profoundly unhealthy neighborhoods, and of how the legacy of racism can literally take years off their lives. Far from being a relic of the past, America’s racist and segregationist history continues to harm black people in the most intimate of ways—seeping into their lungs, their blood, even their DNA.
When Kiarra was a little girl, Baltimore was, as it is today, mired in violence, drugs, and poverty. In 1996, the city had the highest rate of drug-related emergency-room visits in the nation and one of the country’s highest homicide rates.
With her father in and out of jail for robbery and drug dealing, Kiarra and her mother, three siblings, and three cousins piled into her grandmother’s home. It was a joyous but chaotic household. Kiarra describes her grandmother as “God’s assistant”—a deeply religious woman who, despite a house bursting with hungry mouths, would still make an extra dinner for the addicts on the block. Kiarra’s mother, meanwhile, was “the hood princess,” a woman who would do her hair just to go to the grocery store. She was a teen mom, like her own mother had been.
Many facets of Kiarra’s youth—the fact that her parents weren’t together, her father’s incarceration, the guns on the corners—are what researchers consider “adverse childhood experiences,” stressful events early in life that can cause health problems in adulthood. An abnormally large proportion of the children in Baltimore—nearly a third—have two or more aces. People with four or more aces are seven times as likely to be alcoholics as people with no aces, and twice as likely to have heart disease. One study found that six or more aces can cut life expectancy by as much as 20 years. Kiarra had at least six.
She and others I interviewed recall the inner-city Baltimore of their youth fondly. Everyone lived crammed together with siblings and cousins, but people looked out for one another; neighbors hosted back-to-school cookouts every year, and people took pride in their homes. Kiarra ran around with the other kids on the block until her grandma called her in each night at 8 o’clock. She made the honor roll in fifth grade and got to speak in front of the whole class. She read novels by Sister Souljah and wrote short stories in longhand.
Yet Kiarra also describes some jarring incidents. When she was 8, she heard a loud bop bop bop outside and ran out to find her stepbrother lying in the street, dead. One friend died of asthma in middle school; another went to jail, then hanged himself. (Other people I spoke with around Penn North and other recovery facilities had similarly traumatic experiences. It seemed like every second person I met told me they had been molested as a child, and even more said their family members had struggled with addiction.)
Kiarra told me she got pregnant by a friend when she was 12, and gave birth to a boy when she was 13. Within a year, the baby died unexpectedly, and Kiarra was so traumatized that she ended up spending more than a month in a psychiatric hospital. When she came home, her boyfriend physically and sexually abused her. He “slapped me so hard, I was seeing stars,” she said.
She took solace in eating, a common refuge for victims of abuse. One 2013 study of thousands of women found that those who had been severely physically or sexually abused as children had nearly double the risk of food addiction. Kiarra ate “everything, anything,” she said, “mostly bad foods, junk food, pizza,” along with chicken boxes—the fried-chicken-and-fries combos slung by Baltimore’s carryout joints.
At first, she thought the extra weight looked good on her. Then she started feeling fat. Eventually, she said, “it was like, Fuck it. I’m fat.” As her high-school graduation approached, she tried on the white gown she’d bought just weeks earlier and realized that it was already too tight.
Kiarra didn’t know many college-educated people, but she wanted to go to Spelman, a historically black college in Georgia, and join a sorority. Her family talked her out of applying, she said. Instead, she enrolled in one local college after another, but she kept dropping out, sometimes to help her siblings with their children and other times because she simply lost interest. After accumulating $30,000 in student loans, she had only a year’s worth of credits.
So Kiarra put college on hold and worked at Kmart and as a home health aide—solid jobs but, as she likes to say, “not my ceiling.” She longed for a purpose. Sometimes, she had an inkling that she was meant to be an important person; she would picture herself giving a speech to an auditorium full of people. But she remained depressed, stuck, and, increasingly, obese.
She began doing ecstasy, and, later, downing a pint of vodka a day. She remembers coming to her home-health-aide job drunk one time and leaving a patient on the toilet. “Did you forget me?” the woman asked, half an hour later. Kiarra broke down crying.
Soon after, she checked into Penn North for her first try at recovery. This past year’s attempt is her third.

Kiarra lives in Sandtown, the Baltimore neighborhood made famous by the Freddie Gray protests, where heart disease and cancer are the leading killers. (Jared Soares)
Sandtown is 97 percent black, and half of its families live in poverty. Its homicide rate is more than double that of the rest of the city, and last year about 8 percent of the deaths there were due to drug and alcohol overdose. Still, its top killers are heart disease and cancer, which African Americans nationwide are more likely to die from than other groups are.
The way African Americans became trapped in Baltimore’s poorest—and least healthy—neighborhoods mirrors their history in the ghettos of other major cities. It began with outright bans on their presence in certain neighborhoods in the early 1900s and continued through the 2000s, when policy makers, lenders, and fellow citizens employed subtler forms of discrimination.
In the early 1900s, blacks in Baltimore disproportionately suffered from tuberculosis, so much so that one area not far from Penn North was known as the “lung block.” In 1907, an investigator hired by local charities described what she saw in Meyer Court, a poor area in Baltimore. The contents of an outdoor toilet “were found streaming down the center of this narrow court to the street beyond,” she wrote. The smell within one house was “ ‘sickening’ … No provision of any kind is made for supplying the occupants of this court with water.” Yet one cause, the housing investigator concluded, was the residents’ “low standards and absence of ideals.”
When blacks tried to flee to better areas, some had their windows smashed and their steps smeared with tar. In 1910, a Yale-educated black lawyer named George McMechen moved into a house in a white neighborhood, and Baltimore reacted by adopting a segregation ordinance that The New York Times called “the most pronounced ‘Jim Crow’ measure on record.” Later, neighborhood associations urged homeowners to sign covenants promising never to sell to African Americans.
Some of Baltimore’s rowhouses are so long-forsaken, they have trees growing through the windows. They are in themselves harmful to people’s health.
For much of the 20th century, the Federal Housing Administration declined to insure mortgages for blacks, who instead had to buy homes by signing contracts with speculators who demanded payments that, in many cases, amounted to most of the buyer’s income. (As a result, many black families never reaped the gains of homeownership—a key source of Americans’ wealth.) Housing discrimination persisted well beyond the Jim Crow years, as neighborhood associations rejected proposals to build low-income housing in affluent suburbs. In the 1990s, house flippers would buy up homes in Baltimore’s predominantly black neighborhoods and resell them to unsuspecting first-time home buyers at inflated prices by using falsified documents. The subsequent foreclosures are a major reason so many properties in the city sit vacant today.
Some of Baltimore’s rowhouses are so long-forsaken, they have trees growing through the windows. These dilapidated homes are in themselves harmful to people’s health. Neighborhoods with poorly maintained houses or a large number of abandoned properties, for instance, face a high risk of mouse infestation. Every year, more than 5,000 Baltimore children go to the emergency room for an asthma attack—and according to research from Johns Hopkins, mouse allergen is the biggest environmental factor in those attacks.
The allergen, found in mouse urine, travels through the air on dust, and Johns Hopkins researchers have found high levels of it on most of the beds of poor Baltimore kids they have tested. When kids inhale the allergen, it can spark inflammation and mucus buildup in their lungs, making them cough and wheeze. These attacks can cause long-term harm: Children with asthma are more likely to be obese and in overall poorer health as adults. Getting rid of the mice requires sealing up cracks and holes in the house—a process that can cost thousands of dollars, given the state of many Baltimore homes.
The mice, of course, are just one symptom of the widespread neglect that can set in once neighborhoods become as segregated as Baltimore’s are. One study estimated that, in the year 2000, racial segregation caused 176,000 deaths—about as many as were caused by strokes.
All Summer, Penn North’s aging air conditioners strained against the soupy heat outside. For Kiarra, the first few months at the recovery center felt like boot camp. The staff woke the residents before 7 a.m., even if they didn’t have anywhere in particular to be. Kiarra’s days were packed with therapies: acupuncture in the mornings, meant to help reduce cravings; individual meetings with peer counselors; Narcotics Anonymous sessions, in which dozens of strangers slumped on metal folding chairs and told stories of past drug binges.
Once a week, Kiarra would leave her post at the front desk and walk across an empty playground for an appointment with her psychotherapist, Ms. Bea (who asked that I not use her full name). Kiarra would climb the steep, narrow staircase of Penn North’s clinical building, then stop at the landing to catch her breath.
Healing the Divide: Kiarra’s Story
Olga Khazan, Kiarra Boulware, and Steve Dixon, the director of Penn North Recovery, discuss persistent health disparities in Baltimore
Ms. Bea’s goal was to help Kiarra understand how her substance abuse, her weight, and her difficult childhood were interconnected. Like many young people in Baltimore, Kiarra had spent her life trying to attain ordinary things—love, respect—that seemed always to skid beyond her grasp. She wanted male attention, but then she got pregnant. The baby made her happy, but the baby died. Her siblings started having kids and she loved them, but she was jealous. She fell into a deep-sink depression. She’d eat a second dinner, then get so drunk that she’d scream at her friends. She’d realize that she was going to wake up to a blistering hangover and would keep drinking. It was coming anyway, so why not? “Struggle days,” she called these times.
During one appointment in August, Kiarra told Ms. Bea that she had been attending Overeaters Anonymous meetings by phone. Something another member had shared, about why people are sometimes reluctant to shed weight, had stuck with her. “He was saying when you lose the fat, you lose a part of you,” Kiarra recalled.
A few years earlier, she had founded a club for plus-size women called Beautiful Beyond Weight, with some of her best friends. The goal was to help overweight women feel better about themselves. They put on fashion shows that she described as “Beyoncé big, but on a Christina Aguilera budget.” She worried that if she lost too much weight, the other girls in the club would think she was a hypocrite. She decided she would aim to be “slim-thicc”—not too skinny.
“So imagine if you were a size 14,” Ms. Bea said. “What would be happening here—with you?”
Ms. Bea was trying to help Kiarra see how she sometimes uses her size as a form of protection, a way of making her feel invisible to men, so that she could eventually work through her fear.
In Kiarra’s experience, disappearing could be useful. She told me that once, when she was 17, before she had gotten so big, she met a guy in an online chat room. She went over to his place, where they watched TV and started having sex. But then—the skid—his three friends barged into the room and raped her. She fled, half-dressed, as soon as she could.
“Yeah,” Kiarra said, envisioning herself many sizes smaller. “I wouldn’t be able to take it.”
Kiarra has trouble concentrating sometimes, and she thinks the reason might be that she and her brother were exposed to lead from old paint. When Kiarra was 6, her grandmother heard that a girl living in another property owned by the same landlord had been hospitalized. She took Kiarra to get tested. The results showed that the concentration of lead in her blood was more than six times the level the Centers for Disease Control and Prevention considers elevated—an amount that can irreversibly lower IQ and reduce attention span. Kiarra, too, was hospitalized, for a month.
Scientists and industry experts knew in the 19th century that lead paint was dangerous. “Lead is a merciless poison,” an executive with a Michigan lead-paint company admitted in a book in 1892. It “gradually affects the nerves and organs of circulation to such a degree that it is next to impossible to restore them to their normal condition.” But as late as the 1940s and ’50s, trade groups representing companies that made lead products, including the Lead Industries Association, promoted the use of lead paint in homes and successfully lobbied for the repeal of restrictions on that use. Lead-paint companies published coloring books and advised their salesmen to “not forget the children—some day they may be customers.” According to The Baltimore Sun, a study in 1956 found that lead-poisoned children in the slums of Baltimore had six times as much lead in their systems as severely exposed workers who handled lead for a living.
In speeches and publications, Lead Industries Association officials cast childhood lead poisoning as vanishingly rare. When they did acknowledge the problem, they blamed “slum” children for chewing on wood surfaces—“gnaw-ledge,” as Manfred Bowditch, the group’s health-and-safety director, called it—and their “ignorant parents” for allowing them to do so. In a letter to the Baltimore health department, Bowditch called the lead-poisoned toddlers “little human rodents.”
Life expectancy at birth in Baltimore by neighborhood.
Even after stricter regulations came along, landlords in segregated neighborhoods—as well as the city’s own public-housing agency—neglected properties, allowing old paint to chip and leaded dust to accumulate. Some landlords, seeking to avoid the expense of renovating homes and the risk of tenant lawsuits, refused to rent to families with children, since they would face the greatest risk from lead exposure. Poor families feared that if they complained about lead, they might be evicted.
Partly because of Maryland’s more rigorous screening, the state’s lead-poisoning rate for children was 15 times the national average in the ’90s; the majority of the poisoned children lived in the poor areas of Baltimore. In some neighborhoods, 70 percent of children had been exposed to lead. The city’s under-resourced agencies failed to address the problem. Clogged by landlords who hid behind shell companies, Baltimore’s lead-paint enforcement system had ground to a halt by the time Kiarra was poisoned. According to Tapping Into The Wire, a book co-authored by Peter L. Beilenson, the city’s former health commissioner, Baltimore didn’t bring a single lead-paint enforcement action against landlords in the ’90s. (A subsequent crackdown on landlords has lowered lead-poisoning rates dramatically.)
When Kiarra was 14, her family sued their landlord for damages, but their lawyer dropped the case because the landlord claimed he had no money and no insurance with which to compensate them. Kiarra remembers her grandmother not wanting to give up, demanding of the lawyer, “What do you mean there’s nothing you can do?”—only to get lost in a tangle of legal rules she didn’t fully understand.
On a hot Saturday this past August, Kiarra brought her nieces with her to work and corralled them in the front office. She was babysitting that day, and staffing was short at the center. The girls climbed restlessly on the stained office chairs and under the tables.
Kiarra is close with her family. She spends much of her free time texting her favorite sisters on her cracked cellphone, and she talks to her grandmother every few days. Any familial strife upsets her deeply: She can vividly recount a long list of times her mother disappointed her. Then again, sometimes she feels like she’s the one who has let everyone down, with all her drinking and dropping out.
Near the end of the day, Kiarra’s cellphone rang. It was her father, calling to yell at her because she hadn’t come to see him recently. “I’ve been busy,” Kiarra told him.
When Kiarra was little, and when her father wasn’t incarcerated, he had provided for his children—unlike many dads she knew. She’d sought his approval by researching Islam, his religion, and trying to reconcile it with the strict Christianity of her grandmother’s home. A few years ago, she tried to impress him by joining a tough-seeming social club that turned out to be too much like a gang. (It “wasn’t a good fit,” she told me.)
On some level, she still respected her father. But he had an explosive personality and struggled with depression and addiction. Kiarra told me he taught her what men are supposed to be: fierce protectors who sometimes turn their wrath on the women in their lives.
Kiarra usually tried to see her father’s outbursts as a cry for help. But today, she decided to confront him. Their conversation escalated as they accused each other of failing at fatherhood and daughterhood.
“How many of my plays have you been to?,” Kiarra demanded.
Her father launched into a tirade. “I will come for your fucking dumb ass!,” I overheard him yell at one point. “You going to respect me!”
“Respect works both ways,” Kiarra said. “I’m not that little girl that’s gonna let you slap the shit out of me.”
What bothered Kiarra most was that her father had never hit his other daughter that way, so why her? Why did it feel like he was always rejecting her? (Her father later confirmed that he had hit her as a child, saying, “Discipline is a must, whatever form you choose.”)
As he continued screaming—“I’m gonna put your fuckin’ head in the dirt”—Kiarra’s eyes glazed over. “Death gotta be better than here,” she said.
She hung up, then wiped away tears. Just today, he had called her at 12:30 a.m., 3:48 a.m., 7:47 a.m., 11:24 a.m., 3:33 p.m., and 4:44 p.m. One time when she didn’t answer the phone, Kiarra said, he showed up in person at Penn North.
Her father called back, rambling less coherently than before. “How much of my life did you spend incarcerated?,” Kiarra asked him. When she was little, she would go out hustling with him. “I was 14 fucking years old seeing dead fucking bodies, and you’re talking about where the fuck did this drinking shit come from?”
Kiarra hung up, this time for good. Then she wept. “As long as I’m fucked up, this man is cool, but as soon as I decide I want to get my fucking life together it’s like …” Her voice trailed off. She turned and told me she wanted to go to McDonald’s. “McDonald’s is killing me,” she said, “but it’s a special treat.”
She ordered her usual—a McDouble and a McChicken, along with a sweet tea—and waited silently amid the beeping of the cash registers.
Most of the people I met at Penn North were optimistic and surrounded by fiercely loyal friends. But their lives also seemed, like Kiarra’s, unrelentingly stressful. Between the hugs and handshakes, I heard a lot of trepidation. I have to move again … Where will I go? Will I get this job at Target? Will I ever walk again? Will I get to eat today?
Research shows that this kind of day-in, day-out worry can ravage a person’s health. Certain stressful experiences—such as living in a disordered, impoverished neighborhood—are associated with a shortening of the telomeres, structures that sit on the tips of our chromosomes, which are bundles of DNA inside our cells. Often compared to the plastic caps on the ends of shoelaces, telomeres keep chromosomes from falling apart. They can also be a measure of how much a body has been ground down by life.
Some researchers think stress shrinks telomeres, until they get so short that the cell dies, hastening the onset of disease. Different kinds of prolonged emotional strain can affect telomeres. In one study, mothers who had high stress levels had telomeres that were as short as those of a person about a decade older. Another study found that children who spent part of their childhood in Romanian orphanages had telomeres that shortened rapidly.
Even among people making $175,000 a year or more, blacks are more likely to suffer from certain diseases than whites are.
Arline T. Geronimus, an expert on health disparities at the University of Michigan, has found that African Americans have more stress-related wear and tear in their bodies than white people do, and the difference widens with age. By measuring telomere length in hundreds of women, Geronimus estimated that black women were, biologically, about seven and a half years older than white women of the same age.
Unrelenting stress also affects our daily behaviors: Stress causes some people to eat more, especially calorically dense foods, and to sleep less. On average, African Americans get about 40 minutes less sleep each night than white people do. Among women in one recent study, poor sleep alone explained more than half the racial disparity in cardiovascular-disease risk.
Living in a dangerous neighborhood like Sandtown requires a vigilance that can flood the body with adrenaline and cortisol. These hormones are supposed to kick in only long enough for us to get away from an immediate threat. If they trickle through us constantly, they can raise the risk of heart disease and compromise the body’s immune system.
These kinds of changes in body chemistry aren’t limited to people living in poverty. Even well-off black people face daily racial discrimination, which can have many of the same biological effects as unsafe streets. Thomas LaVeist, the dean of Tulane’s School of Public Health and Tropical Medicine, has found, for example, that even among people earning $175,000 a year or more, blacks are more likely to suffer from certain diseases than whites are.
In an emerging field of research, scientists have linked stress, including from prejudice, to compounds called methyl groups attaching to our genes, like snowflakes sticking to a tree branch. These methyl groups can cause genes to turn on or off, setting disease patterns in motion. Recently, a study linked racial discrimination to changes in methylation on genes that affect schizophrenia, bipolar disorder, and asthma.
Several studies also show that experiencing racism might be part of the reason black women are about 50 percent more likely than white women to have premature babies and about twice as likely to have low-birth-weight babies. Researchers think the stress they experience might cause the body to go into labor too soon or to mount an immune attack against the fetus. This disparity, too, does not appear to be genetic: Black women from sub-Saharan Africa and the Caribbean are less likely to have preterm births than African American women are, possibly because they’ve spent less time living in America’s racist environment.

Kiarra Boulware (Jared Soares)
Throughout the fall, Kiarra kept her doctor appointments, and she began working out at the small gym at Penn North, placing a picture of Chrissy Lampkin, the curvaceous girlfriend of the rapper Jim Jones, on her treadmill as motivation.
But Kiarra still wasn’t losing much weight. Like most Americans, she got advice from her friends on what to eat—but that advice at times proved confusing and contradictory. She tried a boiled-egg diet, which left her with hunger pangs and a lot of leftover eggs in the fridge. She went seven days without meat but wound up eating more starches, which sent her blood sugar soaring.
One bright day in late September, Kiarra returned to Bon Secours to see Ebony Hicks, a behavioral-health consultant who, like Kiarra’s doctor, works through Health Care for the Homeless, a Baltimore nonprofit that cares for the very poor. Hicks began by asking Kiarra what her goal was. Kiarra said getting down to an even 200 pounds “would be awesome.” Her weight remained, stubbornly, about 150 pounds higher than that. But she stayed optimistic, writing down Hicks’s aphorisms about needing to be patient and not expecting immediate results—“Anything overnight usually lasts about a night!”—in a notebook she’d brought with her.
Gently, Hicks asked Kiarra what she had eaten that day.
“French fries,” Kiarra said.
“All you’ve had is french fries?,” Hicks asked.
“Mm-hmm.”
It was 3:30 in the afternoon.
They walked to a room across the hall, and Kiarra stepped onto a scale.
“I gained two pounds,” she said quickly, “so now I’m depressed. I eat too much.”
“We have to work on getting you more regularly eating throughout the day,” Hicks said.
Kiarra asked whether “detox tea,” something she’d heard about from a friend, was healthy.
“You can detox with lots of fiber-filled vegetables,” Hicks said.
“What’s that?,” Kiarra asked.
Hicks pulled up a web page describing fruits and vegetables that contain fiber. She listed them off one by one.
Would Kiarra eat avocados?
No.
Coconut? Also no.
“I do eat berries,” Kiarra said. “Let’s put that down.” Kiarra doesn’t know why she dislikes so many fruits and vegetables. Her grandmother cooked healthy meals, putting turkey in big pots of greens for flavor. She had a rule that you could never leave the table without eating your vegetables. Kiarra would fall asleep at the table.
Hicks gamely pressed on. “Peas? You like peas?”
“I think I’m going to throw up,” Kiarra said, grimacing.
“Chickpeas,” Hicks offered. “You ever ate hummus?”
“What is hummus?”
Fried food has long been Kiarra’s legal high—cheap, easily acquired, something to brighten the gloomiest day. It is also one of the few luxuries around.
Predominantly black neighborhoods tend to become what researchers call “food swamps,” or areas where fast-food joints outnumber healthier options. (Food deserts, by contrast, simply lack grocery stores.) One study in New York found that as the number of African Americans who lived in a given area increased, so did the distance to the nearest clothing store, pharmacy, electronics store, office-supply store. Meanwhile, one type of establishment drew nearer: fast-food restaurants.
That’s not a coincidence. After the riots of the 1960s, the federal government began promoting the growth of small businesses in minority neighborhoods as a way to ease racial tensions. “What we need is to get private enterprise into the ghetto, and put the people of the ghetto into private enterprises,” President Richard Nixon said around the time he created the Office of Minority Business Enterprise, in 1969. As Chin Jou, a senior lecturer at the University of Sydney, describes in her book, Supersizing Urban America, fast-food companies were some of the most eager entrants into this “ghetto” market.
Fast-food restaurants spent the next few decades “rushing into urban markets,” as one Detroit News report put it, seeking out these areas’ “untapped labor force” and “concentrated audience.” In the 1990s, the federal government gave fast-food restaurants financial incentives to open locations in inner cities, including in Baltimore. The urban expansion made business sense. “The ethnic population is better for us than the general market,” Sidney Feltenstein, Burger King’s executive vice president of brand strategy, explained to the Miami Herald in 1992. “They tend to have larger families, and that means larger checks.” (Supermarket chains didn’t share this enthusiasm; in part because the widespread use of food stamps causes an uneven flow of customers throughout the month, they have largely avoided expanding in poor areas.)
One reason college graduates live longer, researchers believe, is that education endows people with the sense that they control their own destiny.
Fast-food executives looked for ways to entice black customers. Burger King made ads featuring Shaft. KFC redecorated locations in cities like Baltimore to cater to stereotypically black tastes, and piped “rap, rhythm and blues, and soul music” into the restaurants, Jou writes. “Employees were given new Afrocentric uniforms consisting of kente cloth dashikis.” A study from 2005 found that TV programs aimed at African Americans feature more fast-food advertisements than other shows do, as well as more commercials for soda and candy. Black children today see twice as many soda and candy ads as white children do.
The marketing and franchising onslaught worked, and the diets of low-income people changed dramatically. Before the rise of fast food and processed foods, many low-income black families grew their own food and ate lots of grains and beans. In 1965, one study found, poor and middle-income blacks ate healthier—though often more meager—diets than rich whites did. But over the next few decades, the price of meat, junk food, and simple carbohydrates plummeted, while the price of vegetables rose. By the mid-’90s, 28 percent of African Americans were considered by the U.S. Department of Agriculture to have a “poor” diet, compared with just 16 percent of whites.
At Carver Vocational-Technical High School, which Kiarra and Freddie Gray attended at the same time, only about a third of students go on to enroll in college—yet another factor that could be contributing to the area’s low life expectancy, given that college graduates outlive high-school dropouts in every racial category.
One reason college graduates live longer, researchers believe, is that education endows people with the sense that they control their own destiny. Well-educated people seek out more nutritional information because they’ve been told they can achieve anything—why not perfect health, too?
Kiarra, by contrast, wasn’t yet sure what she could accomplish. She wanted to live up to an image in her mind of a “fly, crazy, daring, dream-chasing girl,” but she cycled between getting excited about new possibilities and being flattened by setbacks. Sometimes, she would dream of turning Beautiful Beyond Weight into a business—one that would sell T-shirts and caps with empowering messages for plus-size women. But she wasn’t really sure how to do that.
When Kiarra felt especially adrift, she would visit Steve Dixon, Penn North’s director, in his tiny office at the end of the hall, and ask him for advice on finding her purpose. He would tell her to pray and meditate. “When you pray, it’s like you’re talking to God,” Kiarra told me once. “But when you meditate, it’s God talking to you.”

Kiarra sometimes asks Steve Dixon, the director of Penn North, for advice on how to find her purpose in life. (Jared Soares)
In November, some combination of prayer, meditation, and research led Kiarra to enroll in a medical-assistant training program. The class added another $7,000 to her student-loan debt, but Kiarra seemed to thrive in it, and a few weeks before Christmas, she was excitedly planning her post–Penn North life. Once she had her medical-assistant certificate in hand, she would move to Philadelphia, get a job at Temple University, and take classes to become a registered nurse. Eventually, she hoped to become a nursing professor. That future held everything she wanted: helping people, being a leader, making her own money, having her own place.
Feeling chipper, she decided to browse the wigs at a nearby store, stroking the hairpieces and whispering to the best ones that she would be back for them on payday. She had a new reason to get dolled up: a truck driver, “fine as wine” and with no kids—and, accordingly, no messy entanglement with another woman. She tried to boss him around, but he told her to mind her own business, and she kind of liked that. His birthday was approaching, and she wanted to take him someplace fancy. She would wear a black dress, and he would wear a black suit.
To help pay for everything, Kiarra decided to register as a Lyft driver. All that was required was a $250 deposit; she began calling around to different relatives to raise the money.
Twenty-seventeen, she thought, had been her best year yet.
A few weeks later, a bitter cold settled through the East Coast, and Kiarra’s sunny mood had faded. Things had ended with the truck driver over some mean Facebook posts and the fact that he’d lied to her about not having kids. She was also reconsidering her plans for the future, now thinking that instead of setting her sights on Temple, she should focus on graduating and finding a job—any job—that would pay well enough and provide insurance that would cover her extensive health-care needs. Her grandmother said driving for Lyft in Baltimore was too dangerous. She might not move to Philly after all.
Kiarra figured that if she really wanted to have a successful plus-size clothing brand, she’d at least have to live long enough to see it happen.
But a new opportunity presented itself. Because of a change in her insurance plan, Kiarra had to switch doctors. Right away, her new doctor asked her whether she had considered bariatric surgery. Kiarra said she was scared of the complications, such as digestive problems and infections, but the doctor reassured her that complications are rare. She was interested in the gastric sleeve, a procedure that would dramatically reduce the size of her stomach, causing hormonal changes that would help her lose much of her body fat.
Kiarra still felt conflicted about losing her identity as an overweight woman. She couldn’t relate to the people on the Overeaters Anonymous calls who said they hated their bodies. She liked hers. “People say, ‘Hey, you’re fat,’ ” she said. “And I’m like, ‘That’s obvious.’ ” But she was motivated by her diabetes—which was already causing her vision to blur and her feet to tingle—along with the looming threat of other “fat diseases,” as she called them, frightening ones like heart failure. She figured that if she really wanted to have a successful plus-size clothing brand, she’d at least have to live long enough to see it happen.
She decided on the spot to go forward with the surgery, worried that she might change her mind otherwise. She signed up for the mandatory pre-op classes that prepare participants to eat just half a cup of food for every meal, at least initially, after the surgery. Her mother was nervous, but her sisters were all for it. Her grandmother told her to put it in God’s hands.
Earlier that month, Kiarra had organized a birthday party for her 2-year-old niece, Brooklynn, in Penn North’s community room, decking out the dingy yellow walls with pink balloons and ribbons. Within a few weeks, it was decided that Kiarra would gain custody of Brooklynn for a while so that Kiarra’s sister could go back to get her high-school diploma.
Kiarra was happy with this arrangement—she already sometimes referred to Brooklynn as her “daughter-girl”—and she began to see Brooklynn as a reason to stay on track. Juggling coursework and single parenthood exhausted her at times, but she wanted to be the successful role model for Brooklynn that she never had herself. In the chatty toddler who loved dress-up and Moana, Kiarra had found, if not her purpose, at least a purpose. “It feels like the Earth is full, you know?” she told me one day this spring.
Her new status as the child’s guardian meant that her stay at Penn North could be extended, through some alchemy of program definitions, for nearly another year. Staying on would mean cheap housing for Kiarra and Brooklynn, two people who desperately needed it.
With that settled, Kiarra turned her attention to the six-month process of hoop-jumping that was required to qualify for the gastric-sleeve surgery. The first pre-op class was an hour and a half long and took place at a hospital 30 minutes from Penn North. Kiarra thought the time commitment seemed excessive; with a smirk, she wondered aloud why the doctors couldn’t just tell her and the other patients, “Y’all fat. We gonna cut you up.”
But the doctors needed Kiarra to understand that the surgery was not something to take lightly. To qualify, she would have to get her sleep apnea and diabetes under control. She would have to keep a food journal, submit to behavioral evaluations, write an essay explaining why she no longer wanted to be morbidly obese. For the rest of her life, she’d need to wait 30 minutes between eating a meal and drinking a beverage. When one of Kiarra’s classmates said that after the surgery, eating too much would cause you to get violently sick for an hour, Kiarra recoiled a little.
All of the rules and obligations seemed more intense than Kiarra had expected. “Six months, you’re going on like 16 appointments,” she said. “Whoo, that’s a lot.” Given all she had to contend with, I wondered whether she would end up meeting the requirements—and, given the stakes, what might happen to her if she didn’t.
Tony Conn, a Penn North staffer with whom Kiarra is close, calls her a “wonderful, brilliant person.” Early on in my reporting, he told me her biggest flaw is that she sometimes doesn’t see things through to the end. “As soon as [something] looks like it’s gonna come to light, she’s like, ‘Okay, I did that. So let’s find something else,’ ” he said.
But lately, Kiarra had shown a new sense of calm and dedication. One day while she worked the front desk, an older man flirted with her as he signed the attendance sheet.
“When you look in the mirror,” he said, “and see how beautiful you are, what do you say to yourself?”
“We’ve come a long way,” she said quietly. “Let’s stay there.”