Shortlisted contenders, from left: Collince Oluoch; Roy Allela; Beth Koiji; Neo Hutiri; Paul Matovu. Photograph: Brett Eloff and James Oatway/Royal Academy of Engineering
Shortlisted contenders for the Royal Academy of Engineering Africa prize reveal their designs, from gloves that translate sign language into speech to smart lockers that dispense medicines.
The Royal Academy of Engineering Africa prize, now in its fifth year, has shortlisted 16 African inventors from six countries to receive funding, training and mentoring for projects intended to revolutionise sectors from agriculture and science to women’s health. The winner will be awarded £25,000 and the three runners up will receive £10,000 each.
From smart gloves that turn sign language into audio speech, to water harvesting systems that change air into drinking water, five inventors on course to transform the continent for the better spoke to the Guardian about their innovations.
Kenya: Sign-IO
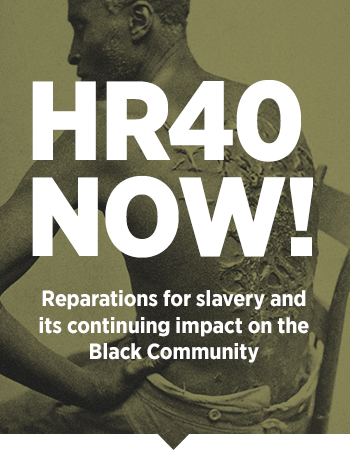
Roy Allela’s six-year-old niece was born deaf. She found it difficult to communicate with her family, none of whom knew sign language. So Allela – a 25-year-old Kenyan technology evangelist who works for Intel and tutors data science at Oxford University – invented smart gloves that convert sign language movements into audio speech.

Roy Allela has developed a glove that translates sign language to speech via a bluetooth-enabled smartphone. Photograph: Brett Eloff/Royal Academy of Engineering
The gloves – named Sign-IO – have flex sensors stitched on to each finger. The sensors quantify the bend of the fingers and process the letter being signed. The gloves are paired via Bluetooth to a mobile phone application that Allela also developed, which then vocalises the letters.
“My niece wears the gloves, pairs them to her phone or mine, then starts signing and I’m able to understand what she’s saying,” says Allela. “Like all sign language users, she’s very good at lip reading, so she doesn’t need me to sign back.”
Allela piloted the gloves at a special needs school in rural Migori county, south-west Kenya, where feedback helped inform one of the most important aspects of the gloves: the speed at which the language is converted into audio.
“People speak at different speeds and it’s the same with people who sign: some are really fast, others are slow, so we integrated that into the mobile application so that it’s comfortable for anyone to use it.”
Users can also set the language, gender and pitch of the vocalisation through the app, with accuracy results averaging 93%, says Allela. Perhaps most importantly, the gloves can be packaged in any style the user wants, whether that’s a princess glove or a Spider-Man one, he says. “It fights the stigma associated with being deaf and having a speech impediment. If the gloves look cool, every kid will want to know why you have them on.”
The gloves recently won the hardware trailblazer award from the American Society of Mechanical Engineers (ASME) and Allela is using the prize money to land more accurate vocal predictions.
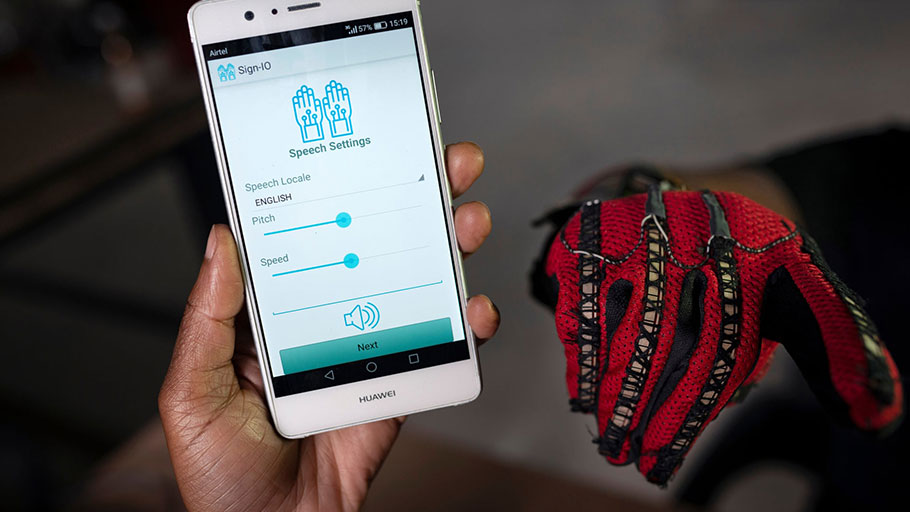
The Sign-IO app, which vocalises words signed by the person wearing the gloves. Photograph: Brett Eloff/Royal Academy of Engineering
His goal is to place at least two pairs of gloves in every special needs school in Kenya, and believes they could be used to help the 34 million children worldwide who suffer disabling hearing loss.
“I was trying to envision how my niece’s life would be if she had the same opportunities as everyone else in education, employment, all aspects of life,” says Allela.
“The general public in Kenya doesn’t understand sign language so when she goes out, she always needs a translator. Picture over the long term that dependency, how much that plagues or impairs her progress in life … when it affects you personally, you see how hard people have it in life. That’s why I’ve really strived to develop this project to completion.”
South Africa: Pelebox smart lockers
When Neo Hutiri was diagnosed with tuberculosis in 2014, the South African engineer was forced to spend three hours every two weeks waiting at his local clinic just to collect his medication. Queuing alongside patients requiring chronic therapy for health issues ranging from cancer to Aids, Hutiri wondered how he could apply technology to the problem and ease the burden for South Africa’s overrun public hospitals.

Neo Hutiri with his Pelebox smart locker, which is designed to cut down the amount of time that patients have to wait for their medication. Photograph: James Oatway/Royal Academy of Engineering
“We have the biggest antiretroviral [ARV] therapy programme in the world: over 4.6m patients receive ARVs and with chronic therapy treatments like this you have to visit the facility every month to receive medication,” says Hutiri.
“It dawned on me that patients are spending a lot of time – 4.3m man hours in total every month – just waiting in queues. So my initial hypothesis was to take patients’ waiting time from three hours to under two minutes.”
Hutiri’s first move was to automate the filing system as much as possible by designing the Pelebox (pele for fast in Setswana), a smart locker that acts as a self-service kiosk. The locker is stocked by health workers, who scan a patient’s medication into a specialised cubicle. The number of the locker and a one-time pin are sent directly to the patient’s mobile phone, with the pin allowing the user to open the locker.
South Africa’s pharmaceutical council was intrigued by the Pelebox, but needed reassurance that the right medications would be delivered to the right patients, every single time. Hutiri piloted the project in Pretoria last year and was overjoyed at the results: 4,700 medications were delivered at a 100% success rate – and with an average collection time of under 36 seconds, says Hutiri.
The 30-year-old entrepreneur has now signed a contract with the department of health to roll the lockers out in eight of South Africa’s nine provinces, a feat he is hugely proud of.
“Eighty-three percent of the South African population relies on state-funded care – my parents are within that population and on long-term medication – but they get short-handed because there isn’t enough of an incentive for entrepreneurs in my sector to serve them as they tend to be low-income,” says Hutiri.
“I wanted to design something that you could place as easily in [the affluent area of] Sandton as in a township. I wanted the product to stand out because then the patients feel a high degree of pride, they think: ‘This product was designed for me’. When you treat people with respect, they pass that respect on to others.”
Uganda: The Vertical Farm
More than two-thirds of Uganda’s population engages in farming, but rapid population growth in the capital, Kampala, means that not everyone who would like to grow their own fruit and veg has the space or land to do so.

Paul Matovu with his Vertical Farm, designed to hold up to 200 plants. Photograph: James Oatway/Royal Academy of Engineering
This was the issue faced by Paul Matovu, who was born into a family of 20 children and raised for a short time by his grandparents in rural Uganda, where he learned all about growing crops. After returning to Kampala as a cash-strapped university student, he began looking for space-saving ways to grow his own food. His solution was the “farm in a box”, a sustainably sourced timber box measuring 90cm wide by 90cm high that can hold up to 200 plants.
The farms currently retail at 300,000 shillings (£64), a high price for the average Ugandan, says Matovu, but as the boxes produce food worth 1.29m shillings (£275) every year, costs can be quickly recouped. The farms also have a wormery in their middle to compost household waste, the castings of which can then be used to fertilise the crops, helping to keep inputs low but still organic, he says.
“Our goal is to roll out the farms to the wealthy, because they do not mind how expensive the boxes are, and to produce three to five farms per day,” says Matovu. “Then we can subsidise sales to the poor.”

The farm boxes have a wormery in their middle to compost household waste, which can then be used to fertilise the crops. Photograph: James Oatway/Royal Academy of Engineering
Kenya: Chanjo Plus
In 2015, Kenyan Collince Oluoch was working as a community health worker in Nairobi, knocking door-to-door to register children for a national immunisation drive. The work was tedious and difficult: every volunteer was required to register 200 children, but because some families were at work or out shopping or had simply moved away, the targets couldn’t always be met.

Collince Oluoch’s mobile platform helps improve the identification and registration of children targeted for life-saving vaccinations. Photograph: Brett Eloff/Royal Academy of Engineering
Oluoch, 27, was faced with a choice: to invent names of children to meet the target (as many other health workers were doing), or to modify the existing pen-and-paper registration system into a digital database. He opted for the latter, and in 2016 built Chanjo Plus, an online vaccination platform that could be accessed by health clinics and hospitals across the country.
“The initial plan was to have an accountable platform to put the faces behind the numbers,” says Oluoch. “We have universal health coverage in Kenya and the aim is that by 2030 we will leave no one behind. But how do you leave no one behind if you don’t even know who everyone is?”
The database uses information compiled by community health workers to build a digital identity for each child, with details on which vaccinations were given and when and where they were given. These records can then be pulled up by any public health clinic anywhere, making it easy to identify which children are falling through the immunisation gaps and provide real-time data on vaccination drives.

Across sub-Saharan Africa, one in five children still don’t have access to life-saving vaccines. Photograph: Brett Eloff/Royal Academy of Engineering
Chanjo Plus has so far enrolled 10,000 children at three clinics in Nairobi, and aims to scale up with the ministry of health to target the 1.5 million children born in Kenya every year, says Oluoch. He then hopes it can be a platform used across sub-Saharan Africa, where one in five children still don’t have access to life-saving vaccines.
“People are still dying because of measles, polio, diarrhoea, and pneumonia – diseases that can be prevented and should not be causing deaths now. Getting every child access to vaccines translates into healthy lives for families: it means poverty reduction and greater access to education.”
Kenya: Majik Water
When Beth Koigi moved into her university dormitory in eastern Kenya, she was horrified that the water coming out of the tap was filthy and laden with bacteria. Within months, she had built her first filter and was soon selling filters to others. When drought hit in 2016 and water restrictions saw Koigi’s water supply turned off entirely, she began thinking about water scarcity and its relation to climate change.

Beth Koigi plans to use her Majik Water innovation to increase access to drinking water among low-income households. Photograph: Brett Eloff/Royal Academy of Engineering
“Going for months without any tap water became a very bad situation,” she says. “Where I used to live, we didn’t get any tap water at all, so even doing simple things like going to the toilet – I would go to the mall instead. Having no water at all is worse than just having unpurified water, so I started thinking about a way to not have to rely on the council.”
While on a four-month programme at the Silicon Valley-based thinktank Singularity University, Koigi, 27, joined up with two other women – American environmental scientist Anastasia Kaschenko and British economist Clare Sewell – to create Majik Water, which captures water from the air and converts it into drinking water using solar technology.
The device – which won first prize this year at the EDF Africa awards – could provide a solution for the 1.8 billion people predicted to have a shortage of water by 2025, according to the UN, says Kaschenko.
“There’s an interesting relationship between climate change and the water in the atmosphere,” she says.
“There’s six times more water in the air than in all the rivers in the world. With every 1F increase in temperature, water begins to evaporate on the ground but increases by about 4% in the atmosphere, and that’s water that’s not being tapped.”

The Majik Water system, which can generate up to 10 litres of filtered water a day. Photograph: Brett Eloff/Royal Academy of Engineering
Majik Water – from the Swahili maji for water and “k” for kuna (harvest) – uses desiccants such as silica gels to draw water from the air. The gels are then heated up with solar power to release the water. The current system can generate up to 10 litres of filtered water per day, with the team looking to scale up to 100-litre systems at a cost of only £0.08 per 10 litres.
The solar panels used for the prototype are the most expensive input on the device, says Koigi, who is looking for ways to drive those costs down.